Overview
This study is the first in Australia to seek strategies to improve safe driving among individuals with chronic pain.
Being able to drive is important and when people stop driving, this can lead to less independence, reduced social integration, lower levels of community participation and poorer quality of life. However, driving is a complex task which requires the ability to quickly identify hazards and react appropriately to avoid crashing.
This study investigated the effect of chronic pain on driving behaviour by:
- Conducting interviews with Australian health professionals and individuals with chronic pain, drawing upon their lived experience
- Comparing the driving behaviour between chronic pain and non-chronic pain (healthy) groups.
The findings highlighted the need for clearer guidelines and educational materials on the impact of chronic pain on an individual’s driving ability. In addition, self-regulation strategies and current barriers and enablers for improving driving were identified from the perspective of individuals with chronic pain, as well as Australian health professionals.
There were no significant differences observed in the hazard perception response time test, self-reported attention- related error and self-reported driving behaviour between the participant groups. However, there were significant differences in the scores of driving lapses, mental demand, physical demand and frustration levels of the driving task.
Overall, the findings contribute to the understanding of current driving behaviours, the challenges for people experiencing chronic pain, and the relationship between chronic pain and driving. The report proposes recommendations and strategies to improve safe driving among people with chronic pain.
Content in this article is drawn from the Royal Automobile Club of Victoria (RACV) funded research project "DRIVING BEHAVIOUR IN PEOPLE WITH CHRONIC PAIN: perspective of people with chronic pain and health professionals". The research was led by Dr Atiyeh Vaezipour from the Technology-enabled rehabilitation team at RECOVER Injury Research Centre.
Dr Vaezipour worked alongside RECOVER colleagues Dr Nicole Andrews and Associate Professor Venerina Johnston as well as collaborators Professor Mark Horswill (UQ School of Psychology), Dr Oscar Oviedo-Trespalacios (CARRS-Q, QUT) and international collaborator Professor Patricia Delhomme (Univ Gustave Eiffel, Université de Paris).
The RACV research will form part of RACV’s submission to the National Transport Commission (NTC) review into its national Assessing Fitness to Drive guidelines. The guidelines, which are used by state authorities including VicRoads to assess a person’s ability to drive, do not currently address chronic pain.
The RACV SAFETY Research Fund "DRIVING BEHAVIOUR IN PEOPLE WITH CHRONIC PAIN – perspective of people with chronic pain and health professionals" Summary Report is available here in downloadable PDF format (PDF, 1.5 MB).
Background
Being able to drive is important and when people stop driving, this can lead to less independence, reduced social integration, lower levels of community participation and poorer quality of life. However, driving is a complex task which requires both the ability to rapidly identify potential hazards and appropriately react to driving situations to avoid crashing. Therefore, attention must be continuously directed towards the road environment as any source of distraction (e.g. talking on a mobile phone, driver pain) could increase the probability of a crash.
Pain could be a source of inattention among drivers, where drivers experiencing pain may present psychological states which could reduce the attentional resources needed to complete the driving task safely. In addition, the type and location of pain could impair functional outcomes such as the movements or reactions needed to control the vehicle safely.
There is a lack of studies investigating the impact of chronic pain on driving behaviour and no evidence to inform evidence-based practice to increase safety among drivers experiencing chronic pain. This study is the first in Australia to seek strategies to improve safe driving among individuals with chronic pain by drawing upon the lived experience of these individuals, as well as the knowledge of health professionals as subject matter experts.
This study investigated the effect of chronic pain on driving behaviour in Australia by:
- Interviewing drivers with chronic pain to identify barriers to safe driving and explore current assessments and treatment offered for driving
- Interviewing Australian health professionals to understand the potential risks associated with chronic pain experience while driving
- Understanding the needs and challenges of adults experiencing chronic pain when they drive using:
- Hazard perception assessments to identify unsafe driving and the difficulties faced while driving
- Self-reported driving crashes/near misses
- Providing recommendations and strategies to improve safe driving among people with chronic pain and assist health professionals to improve the management of driving with chronic pain.
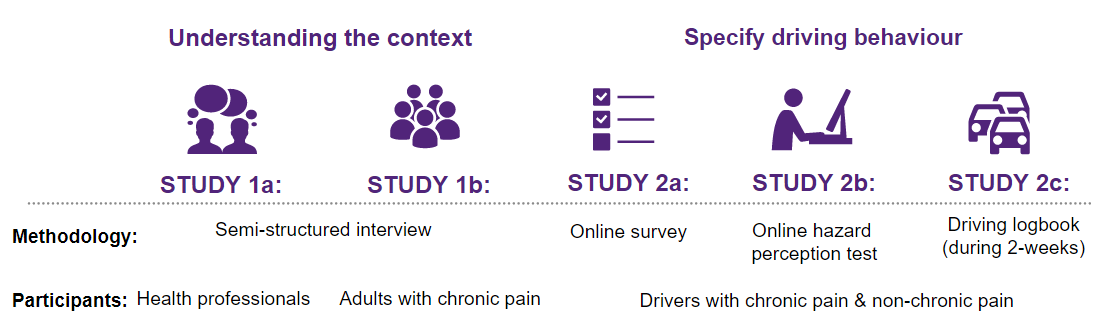
Methodology
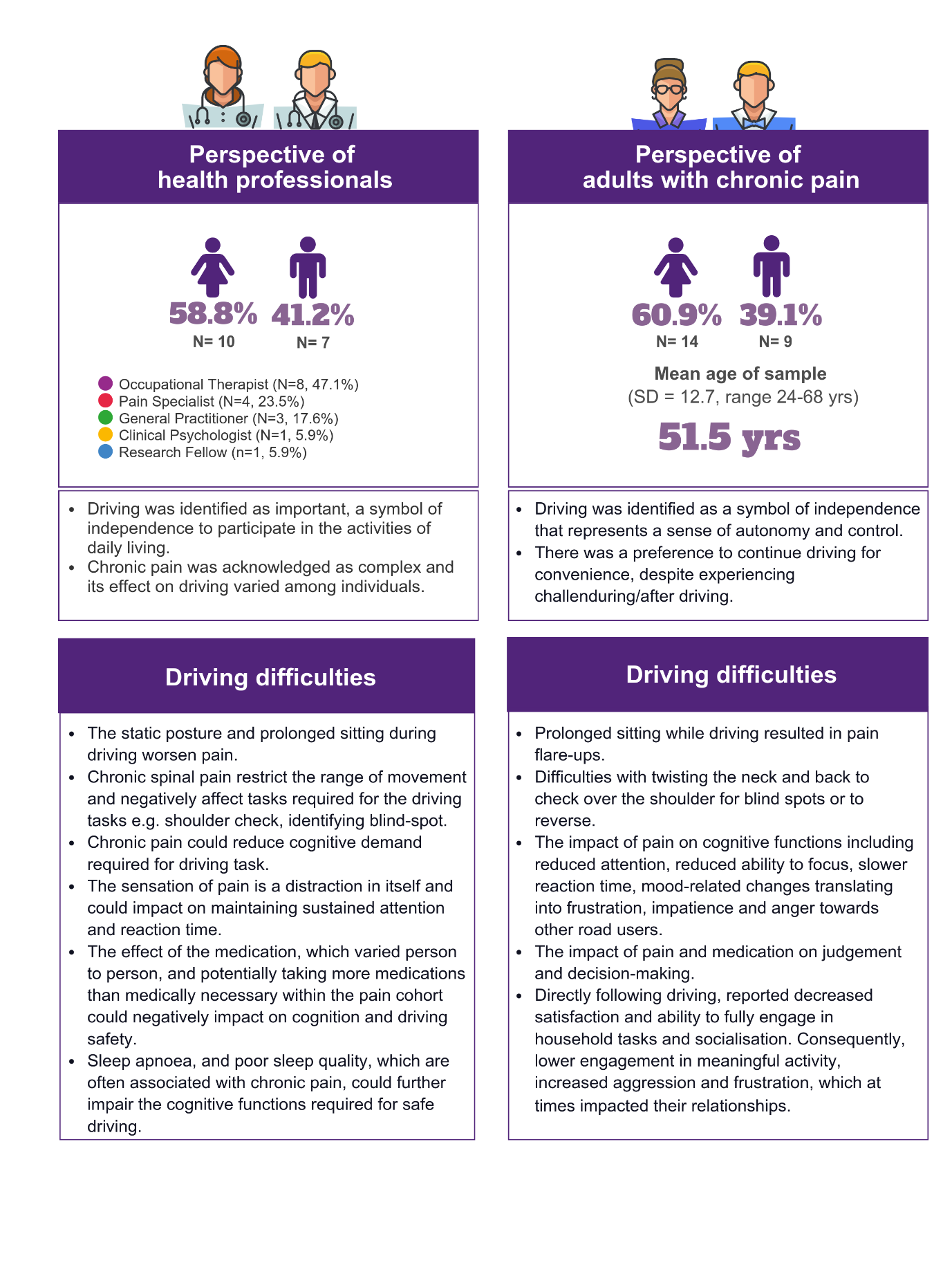
- Interviews were conducted with twenty-three Australian drivers and drew upon their lived experience with chronic pain.
- Seventeen Australian health professionals were interviewed as subject matter experts including occupational therapists (OT), pain specialists, general practitioners (GP), a clinical psychologist and a researcher.
- Self-reported driving behaviours were compared between the chronic pain and non-chronic pain (healthy) participant groups.
- Participants groups completed an anonymous online survey capturing demographics, driving experience, self-reported driving behaviour and pain characteristics.
- A computer-based response-time hazard perception and prediction tests required drivers to view several traffic conflict videos and identify any road users likely to be involved in a traffic conflict as early as possible.
- A driving logbook experiment required drivers to keep a log of their driving over the course of two weeks and self-report their driving experiences. For example, driving workload and near crash events where the driver is required to suddenly manoeuvre the vehicle to
avoid a crash.
Key findings driving behaviour
Ninety participants completed the self-reported online survey and driving logbook study, half were drivers experiencing chronic pain and the other half were otherwise healthy drivers for comparison.
Discussion
Perspectives of health professionals
Health professionals described the GP’s role as collecting comprehensive patient information on physical, cognitive, psychological and neurological conditions. Driving would only be addressed if the patient or family member raised concerns, or if the GP identified that pain could impact driving. If this assessment was made by the GP, the person would be referred to an OT driving assessor for further assessment.
If driving-related concerns were raised by a patient with chronic pain, health professionals worked with them to address the physical, cognitive and emotional aspects related to safe driving. The health professionals would provide several self- regulation strategies according to the challenges identified.
These included utilising activity pacing principals for driving, providing biomechanical and postural adaptations, cushions or vehicle modifications, and coaching drivers to actively scan their environment to identify road hazards as early as possible.
Clinicians encouraged patients to be cautious with medications, particularly new medications or a change in dosage. A small number of clinicians aimed to educate patients on chronic pain and utilised interviewing strategies to increase patient awareness and insight regarding the challenges they may be facing. If driving concerns were out of their scope of practice, patients were referred to their GP, an OT, or a pain management clinic.
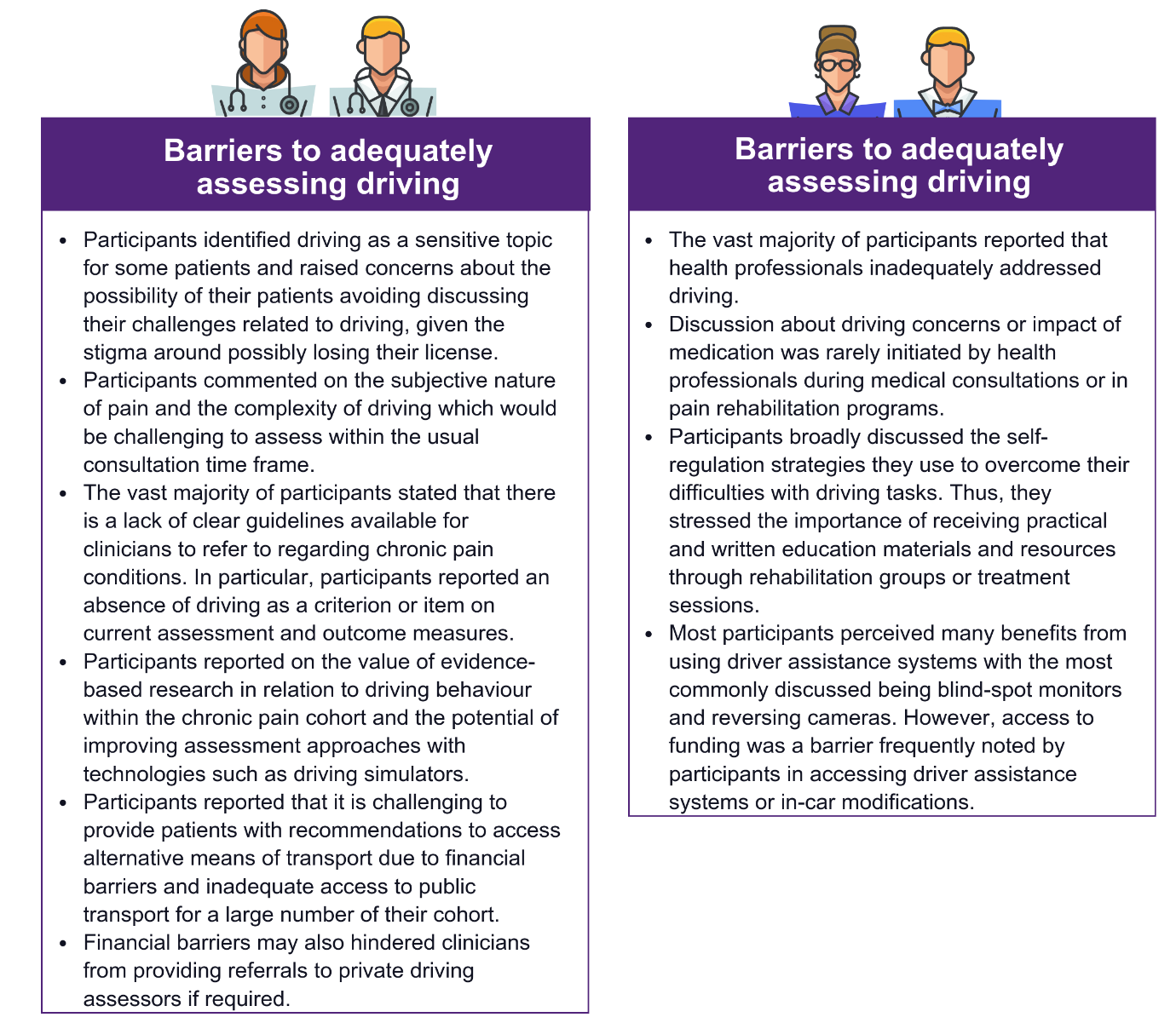
Barriers to assess driving
- Health professionals thought patients avoided discussing their challenges related to driving due to the stigma around possibly losing their licence. They raised awareness of the factors that potentially impact on driving safety and management strategies in an attempt to overcome this barrier.
- Most stated there is a lack of clear guidelines available for clinicians to refer to. They described an absence of driving as a criterion on current assessment and outcome measures.
- Training and upskilling of clinicians was needed in order to better address driving related concerns and understand the impacts of various medication on driving behaviour.
- The subjective nature of pain and the complexity of driving meant it was challenging to assess within a short time frame. This highlights a need for collaboration between pain clinics, GP’s and transport authorities to identify at-risk drivers and continuity of care for the individuals.
- Evidence-based research in relation to driving behaviour within the chronic pain cohort was seen to be valuable and have the potential of improving assessment approaches with technologies such as virtual reality driving simulators.
- It was challenging to provide patients with recommendations to access alternative means of transport or private assessors due to financial barriers and inadequate access to public transport for many patients.
- Addressing funding issues within public health is important to help clinicians to address the multiple challenges faced by chronic pain patients.
- The role of the patient’s family was deemed important to assess a patient’s capacity to drive. There is a need to provide educational materials to the support network of the individual to assess physical, emotional and cognitive components. This would assist with making informed decisions regarding safety to drive.
- Driver assisting technologies could potentially improve driver safety and mitigate some of the driving challenges.
Perspectives of drivers with chronic pain
Interviews involving individuals with chronic pain found that participants viewed driving as a form of independence, which provided a sense of autonomy and control. Participants generally preferred to continue driving for the added convenience, despite the challenges they would experience during/after driving.
Overall, the chronic pain cohort’s reported difficulties with driving included:
- Prolonged sitting resulted in pain flare-ups.
- Difficulties with twisting of the neck and back for head checks (blind spot) or to reverse.
- Impaired cognitive function due to pain including; reduced attention, poorer focus, slower reaction time, and mood-related changes which translated into agitation, frustration, impatience and anger towards other road users. A small number of participants also queried their judgement and decision-making due to the impact of pain and medication.
- Following driving, participants increasingly reported lower satisfaction in several life domains, e.g. being unable to engage fully in household tasks, socialisation or have a restful sleep. Consequently, participants reported lower engagement in meaningful activity, increased agitation, aggression and frustration, which at times impacted their relationships.
Self-regulation strategies included:
- Accepting limitations imposed by pain by making lifestyle changes including reducing the length of time spent driving.
- Asking family members to drive or accompany them.
- Utilising pacing strategies to break up the journey.
- Adding postural supports to increase comfort.
- Using driver assistance systems such as reversing cameras, cruise control and blind-spot monitors.
- Using mindfulness and distraction techniques to overcome the pain.
- Scanning more frequently, maintaining larger spaces between cars and using whole body movements to perform safety checks.
- Utilising avoidance strategies such as avoiding driving due to pain flare-ups, avoiding unnecessary lane changes, high volume traffic, heavy rain and night-time driving.
More than half of the participants reported confidence in their self-assessment by monitoring physical and emotional cues, and four raised concerns about their potential impact on other road users and were mindful of their capacity before driving. A smaller number did not feel that pain negatively impacted their driving safety and did not routinely check whether it was safe for them to drive. However, all expressed interest in gaining more awareness about tools and strategies they can use to gauge their driving safety.
There were mixed perceptions of the impact medications had on driving. A large portion reported self-awareness regarding potential side-effects attributable to their medications. Side-effects included fatigue or sudden onset of drowsiness, reduced concentration and difficulties with sustained attention, diminished coordination and vision issues. A small number reported Tramadol and Valium impaired driving capacity. Management strategies to overcome side effects were discussed, such as reducing dosage, avoiding driving while taking stronger medications or pulling over if required.
Most participants reported that health professionals inadequately addressed driving. Discussion about driving concerns or impact of medication was rarely initiated by health professionals during medical consultations or in pain rehabilitation programs. A small number believed their concerns about driving difficulties would be addressed if it was pertinent to them. Most were in favour of having driving addressed as part of their rehabilitation, given its importance.
Participants broadly discussed recommendations to improve driving assessment and interventions for people experiencing chronic pain. They stressed the importance of receiving practical and written education materials and resources through rehabilitation groups or treatment sessions. In addition, they discussed the importance of clinicians broaching the topic of driving in the context of their pain pathology and medications.
Most participants perceived many benefits to driver assistance systems, the most common being blind-spot monitors and reversing cameras. Access to funding was frequently noted as a barrier in accessing these systems or in-car modifications. Participants also believed that transport authorities could play a role in the assessment of driving safety in chronic pain individuals.
Driving behaviour - self-reported survey and driving logbook
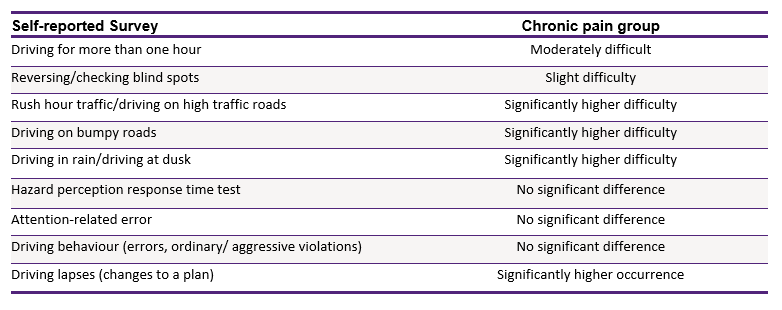
The chronic pain group reported moderate levels of difficulty when driving more than one hour, and a slight level of difficulty in reversing and checking blind spots. They also reported difficulties in certain driving situations including driving in rush hour traffic, driving on high traffic roads, driving on a bumpy road, driving in rain and driving at dusk. These self-reported difficulties were significantly higher compared to the healthy group. Some other findings concerning driver behaviour include:
- No significant differences between groups for self-reported driving behaviour, i.e. errors, ordinary violations and aggressive violations. The only significant difference observed was in the score of lapses which are defined as alterations or unexpected deviations from a properly conceived plan. These are different from mistakes which typically occur because of lack of experience (or expert knowledge) on a driving task. In this research, drivers experiencing chronic pain reported more lapses. Pain could result in different cognitive states which could reduce attention related to the driving task.
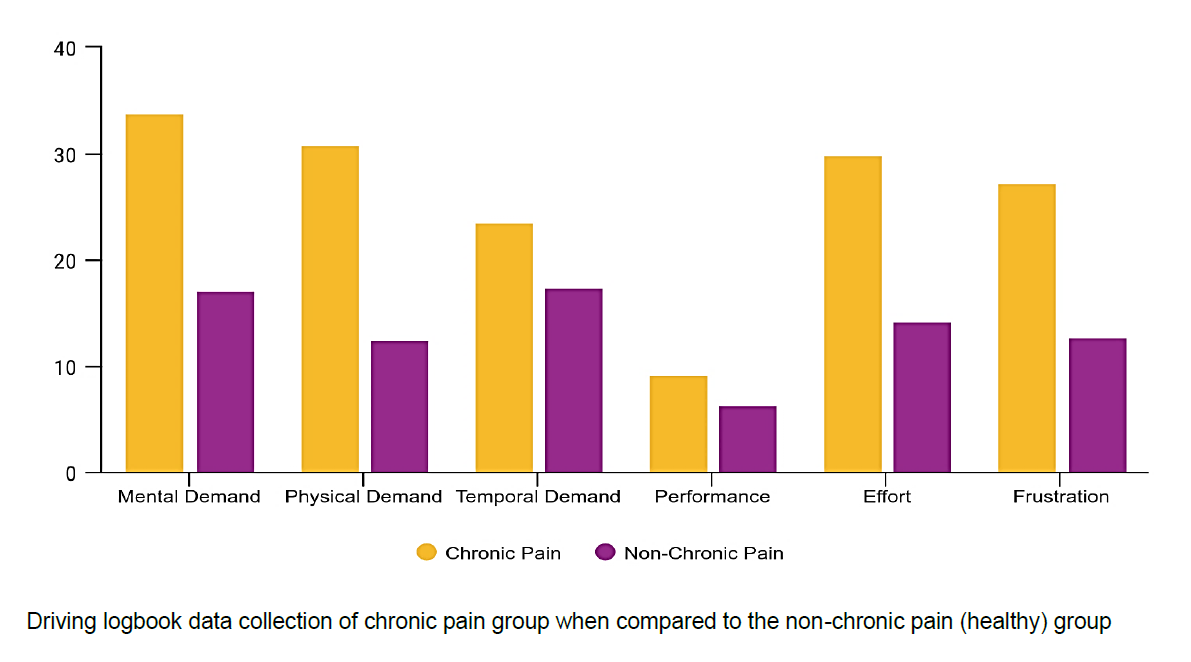
- In relation to the workload of the driving tasks for the driving logbook data collection, there were significant differences in mental demand, physical demand and frustration levels between groups. However, there were no significant differences observed in overall performance and temporal levels of driving tasks. In this research, drivers experiencing chronic pain reported higher levels of perceived mental and physical workload compared to the healthy group. This is consistent with the expectation that pain could influence psychological and functional outcomes of individuals.
- No significant differences between groups in self-reported susceptibility to driver distraction scale, i.e. involuntary distraction. However, there were significant differences in the engagement distraction. Drivers experiencing chronic pain reported less engagement in distracted driving. This further confirms that pain could be a distraction itself, which decreases drivers’ capability to deal with driving demands. Drivers who engage in distracted driving generally negotiate their capability and the driving demands to reduce risks. Therefore, drivers with chronic pain are less likely to engage in additional distractions. Driver inattention taxonomies have consistently reported that mental state can serve as a source of internal distraction, which might make it challenging for the driver to meet the demands of the driving task.
- No significant differences between groups in self-reported attention related errors when driving. These findings can be explained based on the nature of the attention related errors. These are personality trait-like variables, a distinguishable feature of an individual, and seem to reflect on enduring behaviour patterns. Therefore, it is reasonable to think that the presence of chronic pain would have not influenced them.
- Participant groups in this study reported low aggressive responses to anger while driving and there were no significant differences in self-reported driver anger expression –adaptive/ constructive, personal physical aggressive expression, verbal aggressive expression, and the use of the vehicle to express anger.
- No significant differences in hazard perception test response times and predictions made in the hazard prediction test between groups.
- No significant differences between groups in the self- reported number of near misses during the two-week data collection. This could be a consequence of the use of self- regulatory strategies or the fact that driving patterns has been changed as a response to the COVID-19 pandemic.
- Interestingly, although interview participants highlighted the importance of driver assistance system use for individuals with chronic pain, our findings found a limited number own these features in their vehicle. Rear view cameras were the most frequent (26.7%) followed by in-car display (12.2%), and cruise control (8.9%). Clearly there is a need to study acceptability and barriers for the uptake of advanced driver assistant technologies among at-risk groups of drivers.
Recommendations
- Health professionals would benefit from establishing clear and evidence-based guidelines specific for chronic pain, such as Assessing Fitness to Drive as a stand-alone recognised health condition. This could support clinicians with clear recommendations and intervention pathways.
- Health professionals would benefit from training and upskilling to gain confidence to better address medical, physical, emotional and cognitive driving-related concerns since pain is so subjective and complex.
- Health professionals should take a positive approach to raising awareness among individuals experiencing chronic pain on the factors that potentially impact on driving safety (i.e. medications, physical, cognitive, emotional) and management strategies to address these factors.
- While people experiencing chronic pain self-regulate their driving, they could benefit from personalised OT and physiotherapy recommendations on vehicle ergonomics, an ergonomic assessment of their car seating, and educational strategies to reduce pain flare-ups while driving.
- Family members could be included in open discussions about driving to facilitate problem-solving among the clinician, patient and family member.
- People with chronic pain should review their medications with their GP regularly to reduce the harm or compounding effect as a result of taking multiple medications.
- Where possible, if feeling unsafe to drive, supports from family/friends or transport alternatives should be used, e.g. public transport or ridesharing. Road authorities should also continue working towards a more equitable transport system (i.e. accessible public transport, better active travel infrastructure, etc.) to offer viable alternatives to driving.
Links to publications
The full RACV SAFETY Research Fund Report "Driving behaviour in people with chronic pain – perspective of people with chronic pain and health professionals" is available here in downloadable PDF format (PDF, 8.2 MB).